Designing for Neurodiverse Patients
Neurodiversity is a concept that acknowledges the brain differences in individuals, which contribute to diverse ways that people learn and think. Patients who are neurodiverse include those who are Autistic, dyslexic patients, those who have ADD/ADHD, patients affected by traumatic brain injury, as well as those who have Tourette’s Syndrome and other neurocognitive conditions. The healthcare industry is increasingly recognizing the impact of neurodiversity, acknowledging that patients with these conditions may perceive and respond to healthcare environments differently. Sensory processing issues, a common challenge, can lead to challenges, including sensory overload. Recently diagnosed with ADHD, my interest in neurodiversity stems from personal experiences, but also from the stories shared with me by neurodivergent friends.
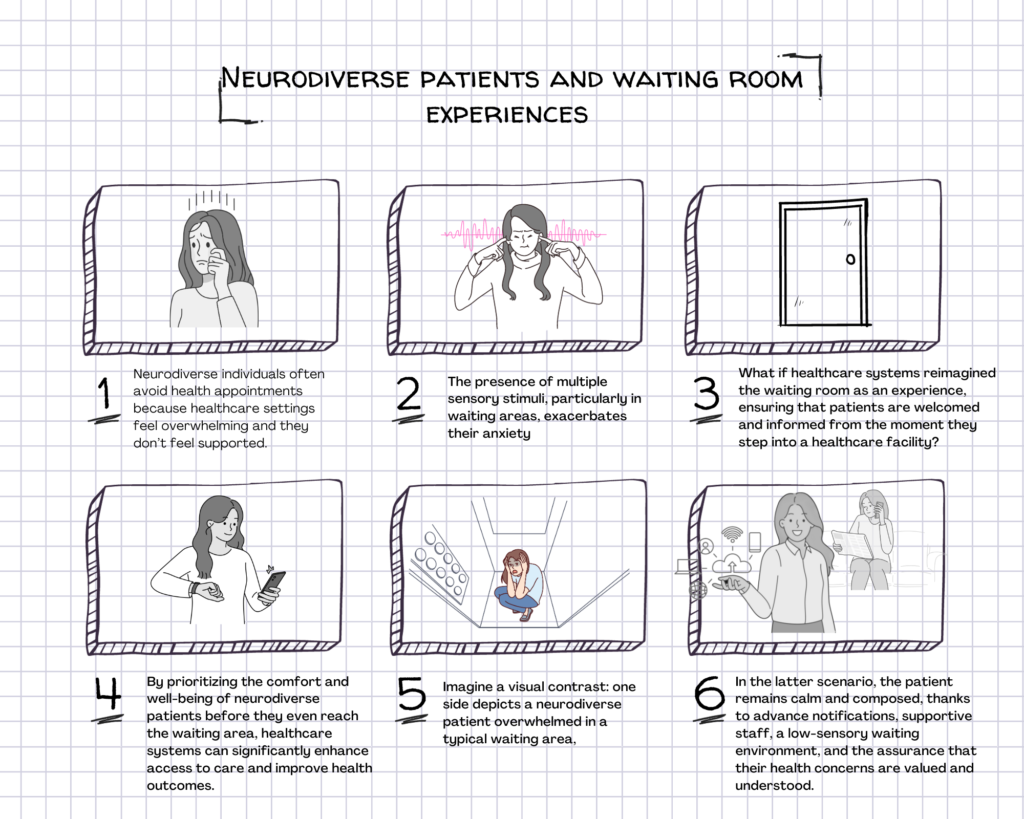
Neurodiversity and the Healthcare Journey: Healthcare organizations are acknowledging the importance of neurodiversity, yet there is a gap in fully implementing strategies to support neurodiverse patients throughout their healthcare journey, including during visits. Many neurodiverse individuals delay seeking health services due to the stress and anxiety associated with healthcare visits, highlighting the need for a reevaluation of patient engagement strategies within healthcare organizations. My goal was to envision a more comprehensive approach, starting from the moment patients enter the healthcare facility.
Where the Journey Begins: While healthcare organizations recognize neurodiversity, this awareness is not consistently reflected in the patient care experience and service design. It is essential to reconfigure various points of contact to minimize stress and anxiety for neurodiverse individuals. I embarked on reimagining how healthcare organizations can effectively guide and support neurodiverse patients from the beginning of their healthcare visit. To delve deeper, I conducted interviews with neurodiverse patients, seeking insights into their primary challenges and experiences within clinical settings. These interviews led to a shift from my initial focus on clinic design. While clinic design does impact patient stress and anxiety, participants revealed that their concerns often originate before a clinical visit.
Support Starts at Home: The anticipation of potential difficulties or challenges in the clinical setting effectively extends the boundaries of the clinical experience into a patient’s home. It became apparent that without support starting at home, patients enter health facilities already feeling vulnerable. When faced with a clinical setting lacking support or services for neurodivergent patients, individuals explained that they feel predisposed to experience anxiety and stress throughout their visits.
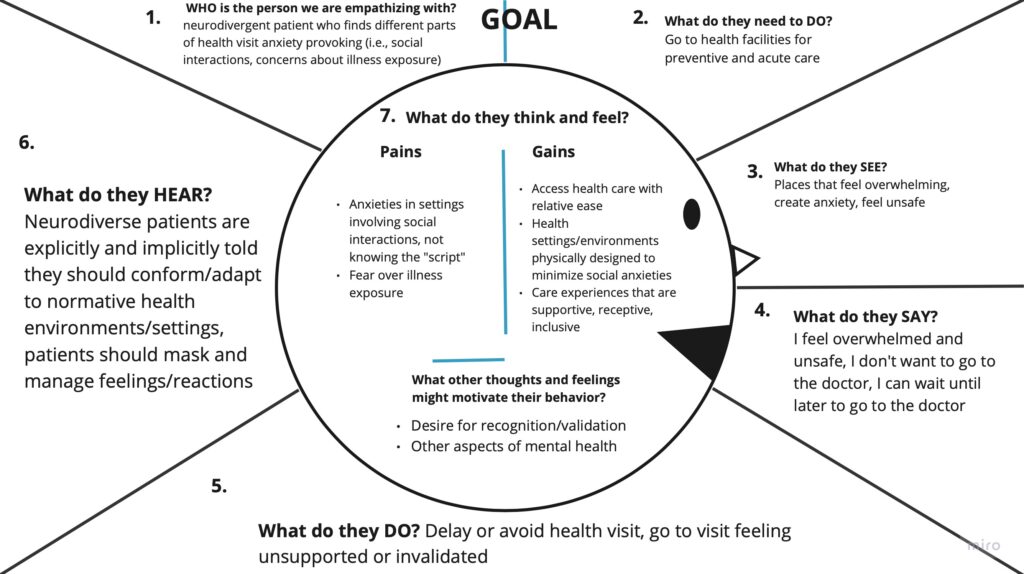
I sought to gain deeper insights from stories participants shared in interviews with me.
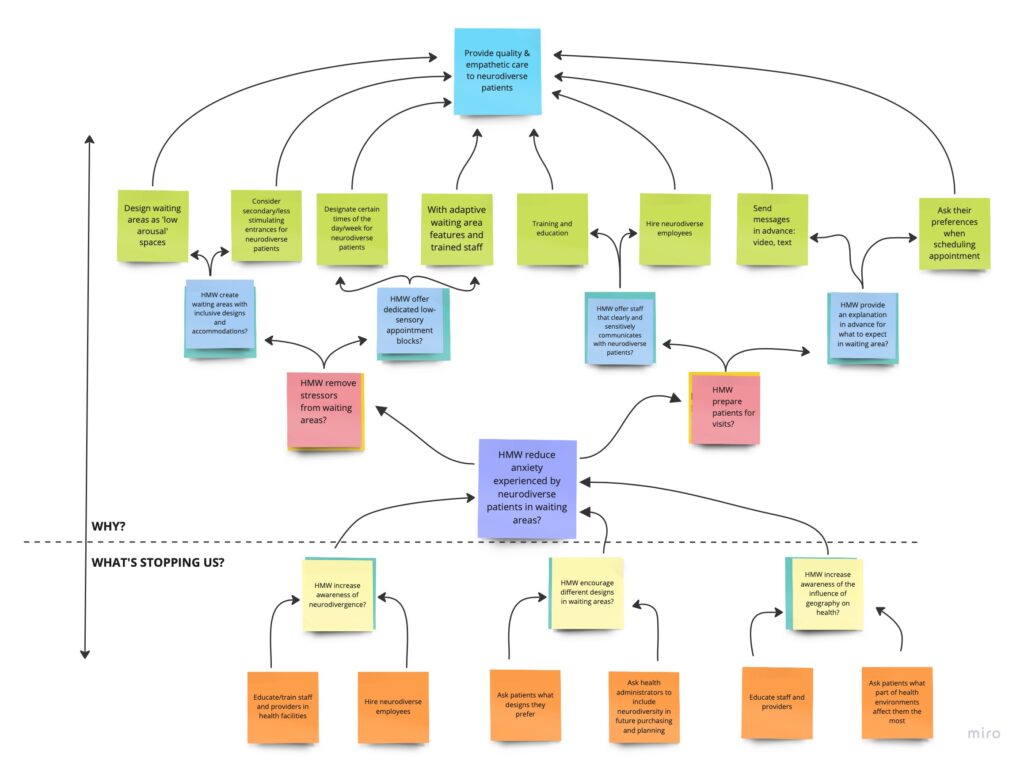
These insights helped guide the next steps…
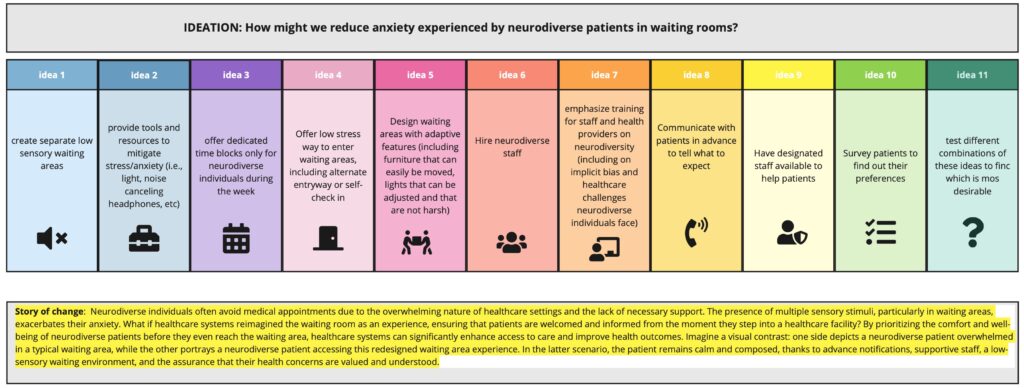
Ideation
Storyboarding